Traumatic Cataract: Background, Pathophysiology, Epidemiology
Traumatic Cataract: Background, Pathophysiology, Epidemiology
Traumatic cataracts occur secondary to blunt or penetrating ocular trauma. Infrared energy (glass-blower's cataract), electric shock, and ionizing radiation are other rare causes of traumatic cataracts.
Cataracts caused by blunt trauma classically form stellate- or rosette-shaped posterior axial opacities that may be stable or progressive, whereas penetrating trauma with disruption of the lens capsule forms cortical changes that may remain focal if small or may progress rapidly to total cortical opacification.
Note the images below.
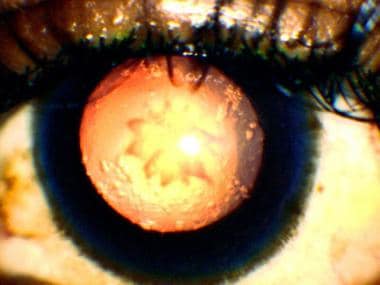
 Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury.
Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury.
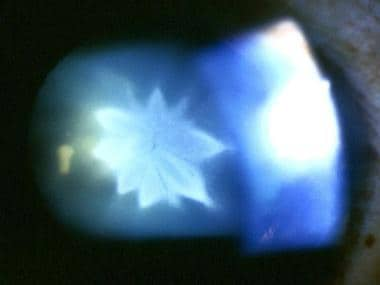
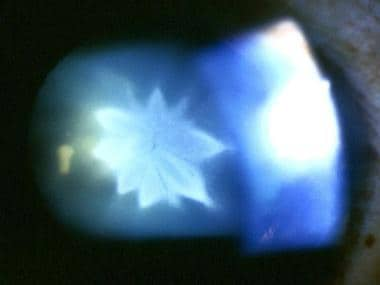
 Same cataract as seen in previous image, viewed by retroillumination.
Same cataract as seen in previous image, viewed by retroillumination.
See What the Eyes Tell You: 16 Abnormalities of the Lens, a Critical Images slideshow, to help recognize lens abnormalities that are clues to various conditions and diseases.
Lens dislocation and subluxation are commonly found in conjunction with traumatic cataract. Other associated complications include phacolytic, phacomorphic, pupillary block, and angle-recession glaucoma; phacoanaphylactic uveitis; retinal detachment; choroidal rupture; hyphema; retrobulbar hemorrhage; traumatic optic neuropathy; and globe rupture.
Traumatic cataract can present many medical and surgical challenges to the ophthalmologist. Careful examination and a management plan can simplify these difficult cases and provide the best possible outcome.
Blunt trauma is responsible for coup and contrecoup ocular injury. Coup is the mechanism of direct impact. It is responsible for Vossius ring (imprinted iris pigment) sometimes found on the anterior lens capsule following blunt injury. Contrecoup refers to distant injury caused by shockwaves traveling along the line of concussion.
When the anterior surface of the eye is struck bluntly, there is a rapid anterior-posterior shortening accompanied by equatorial expansion. This equatorial stretching can disrupt the lens capsule, zonules, or both. Combination of coup, contrecoup, and equatorial expansion is responsible for formation of traumatic cataract following blunt ocular injury.
Penetrating trauma that directly compromises the lens capsule leads to cortical opacification at the site of injury. If the rent is sufficiently large, the entire lens rapidly opacifies, but when small, cortical cataract can seal itself off and remain localized.
United States
Approximately 2.5 million eye injuries occur annually in the United States. It is estimated that approximately 4-5% of a comprehensive ophthalmologist's patients are seen secondary to ocular injury. Traumatic cataract may present as acute, subacute, or late sequela of ocular trauma.
Trauma is the leading cause of monocular blindness in people younger than 45 years. Annually, approximately 50,000 people are left unable to read newsprint as a result of ocular trauma. Only 85% patients who experience anterior segment injury reach a final visual acuity of 20/40 or better, whereas only 40% patients with posterior segment injury reach this level.
The male-to-female ratio in cases of ocular trauma is 4:1.
Work- and sports-related eye injuries most commonly occur in children and young adults. Between 1985-1991, a National Eye Trauma System study reported a median age of 28 years in 648 assault-related cases.
Clinical Presentation
Robert H Graham, MD Consultant, Department of Ophthalmology, Mayo Clinic, Scottsdale, Arizona
Robert H Graham, MD is a member of the following medical societies: American Academy of Ophthalmology, Arizona Ophthalmological Society, American Medical Association
Disclosure: Partner received salary from Medscape/WebMD for employment.
Coauthor(s)
Brian C Mulrooney, MD Private Practice, Ophthalmology, Crestwood Hospital
Brian C Mulrooney, MD is a member of the following medical societies: American Academy of Ophthalmology
Specialty Editor Board
Simon K Law, MD, PharmD Clinical Professor of Health Sciences, Department of Ophthalmology, Jules Stein Eye Institute, University of California, Los Angeles, David Geffen School of Medicine
Simon K Law, MD, PharmD is a member of the following medical societies: American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, American Glaucoma Society
J James Rowsey, MD Former Director of Corneal Services, St Luke's Cataract and Laser Institute
J James Rowsey, MD is a member of the following medical societies: American Academy of Ophthalmology, American Association for the Advancement of Science, American Medical Association, Association for Research in Vision and Ophthalmology, Florida Medical Association, Sigma Xi, Southern Medical Association, Pan-American Association of Ophthalmology
Chief Editor
Hampton Roy, Sr, MD Associate Clinical Professor, Department of Ophthalmology, University of Arkansas for Medical Sciences
Hampton Roy, Sr, MD is a member of the following medical societies: American Academy of Ophthalmology, American College of Surgeons, Pan-American Association of Ophthalmology
Richard W Allinson, MD Associate Professor, Department of Ophthalmology, Texas A&M University Health Science Center; Senior Staff Ophthalmologist, Scott and White Clinic
Richard W Allinson, MD is a member of the following medical societies: American Academy of Ophthalmology, American Medical Association, Texas Medical Association
References
Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury.
Same cataract as seen in previous image, viewed by retroillumination.
Background
Traumatic cataracts occur secondary to blunt or penetrating ocular trauma. Infrared energy (glass-blower's cataract), electric shock, and ionizing radiation are other rare causes of traumatic cataracts.
Cataracts caused by blunt trauma classically form stellate- or rosette-shaped posterior axial opacities that may be stable or progressive, whereas penetrating trauma with disruption of the lens capsule forms cortical changes that may remain focal if small or may progress rapidly to total cortical opacification.
Note the images below.
 Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury.
Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury. 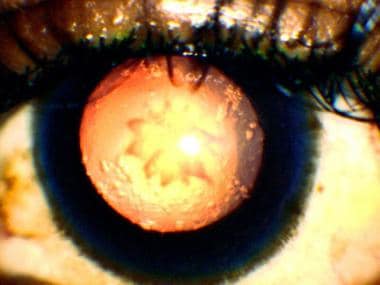 Same cataract as seen in previous image, viewed by retroillumination.
Same cataract as seen in previous image, viewed by retroillumination. See What the Eyes Tell You: 16 Abnormalities of the Lens, a Critical Images slideshow, to help recognize lens abnormalities that are clues to various conditions and diseases.
Lens dislocation and subluxation are commonly found in conjunction with traumatic cataract. Other associated complications include phacolytic, phacomorphic, pupillary block, and angle-recession glaucoma; phacoanaphylactic uveitis; retinal detachment; choroidal rupture; hyphema; retrobulbar hemorrhage; traumatic optic neuropathy; and globe rupture.
Traumatic cataract can present many medical and surgical challenges to the ophthalmologist. Careful examination and a management plan can simplify these difficult cases and provide the best possible outcome.
Pathophysiology
Blunt trauma is responsible for coup and contrecoup ocular injury. Coup is the mechanism of direct impact. It is responsible for Vossius ring (imprinted iris pigment) sometimes found on the anterior lens capsule following blunt injury. Contrecoup refers to distant injury caused by shockwaves traveling along the line of concussion.
When the anterior surface of the eye is struck bluntly, there is a rapid anterior-posterior shortening accompanied by equatorial expansion. This equatorial stretching can disrupt the lens capsule, zonules, or both. Combination of coup, contrecoup, and equatorial expansion is responsible for formation of traumatic cataract following blunt ocular injury.
Penetrating trauma that directly compromises the lens capsule leads to cortical opacification at the site of injury. If the rent is sufficiently large, the entire lens rapidly opacifies, but when small, cortical cataract can seal itself off and remain localized.
Epidemiology
Frequency
United States
Approximately 2.5 million eye injuries occur annually in the United States. It is estimated that approximately 4-5% of a comprehensive ophthalmologist's patients are seen secondary to ocular injury. Traumatic cataract may present as acute, subacute, or late sequela of ocular trauma.
Mortality/Morbidity
Trauma is the leading cause of monocular blindness in people younger than 45 years. Annually, approximately 50,000 people are left unable to read newsprint as a result of ocular trauma. Only 85% patients who experience anterior segment injury reach a final visual acuity of 20/40 or better, whereas only 40% patients with posterior segment injury reach this level.
Sex
The male-to-female ratio in cases of ocular trauma is 4:1.
Age
Work- and sports-related eye injuries most commonly occur in children and young adults. Between 1985-1991, a National Eye Trauma System study reported a median age of 28 years in 648 assault-related cases.
Clinical Presentation
Robert H Graham, MD Consultant, Department of Ophthalmology, Mayo Clinic, Scottsdale, Arizona
Robert H Graham, MD is a member of the following medical societies: American Academy of Ophthalmology, Arizona Ophthalmological Society, American Medical Association
Disclosure: Partner received salary from Medscape/WebMD for employment.
Coauthor(s)
Brian C Mulrooney, MD Private Practice, Ophthalmology, Crestwood Hospital
Brian C Mulrooney, MD is a member of the following medical societies: American Academy of Ophthalmology
Specialty Editor Board
Simon K Law, MD, PharmD Clinical Professor of Health Sciences, Department of Ophthalmology, Jules Stein Eye Institute, University of California, Los Angeles, David Geffen School of Medicine
Simon K Law, MD, PharmD is a member of the following medical societies: American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, American Glaucoma Society
J James Rowsey, MD Former Director of Corneal Services, St Luke's Cataract and Laser Institute
J James Rowsey, MD is a member of the following medical societies: American Academy of Ophthalmology, American Association for the Advancement of Science, American Medical Association, Association for Research in Vision and Ophthalmology, Florida Medical Association, Sigma Xi, Southern Medical Association, Pan-American Association of Ophthalmology
Chief Editor
Hampton Roy, Sr, MD Associate Clinical Professor, Department of Ophthalmology, University of Arkansas for Medical Sciences
Hampton Roy, Sr, MD is a member of the following medical societies: American Academy of Ophthalmology, American College of Surgeons, Pan-American Association of Ophthalmology
Richard W Allinson, MD Associate Professor, Department of Ophthalmology, Texas A&M University Health Science Center; Senior Staff Ophthalmologist, Scott and White Clinic
Richard W Allinson, MD is a member of the following medical societies: American Academy of Ophthalmology, American Medical Association, Texas Medical Association
References
- Tasman W, Jaeger EA. Traumatic cataract. Duane's Clinical Ophthalmology. 1997. 1: 13-4.
- Dinakaran S, Kayarkar VV. Traumatic retinal break from a viscoelastic cannula during cataract surgery. Arch Ophthalmol. 2004 Jun. 122(6):936. [Medline].
- Jaffe NS, Jaffe MS, Jaffe GF. Lens displacement. Cataract Surgery and Its Complications. 1997. 200-11.
- Sarikkola AU, Sen HN, Uusitalo RJ, Laatikainen L. Traumatic cataract and other adverse events with the implantable contact lens. J Cataract Refract Surg. 2005 Mar. 31(3):511-24. [Medline].
- Kanski JJ. Clinical Ophthalmology: A Systematic Approach. 1989. 257-8.
- Shah MA, Shah SM, Shah SB, Patel CG, Patel UA. Morphology of traumatic cataract: does it play a role in final visual outcome?. BMJ Open. 2011 Jan 1. 1(1):e000060. [Medline]. [Full Text].
- Schwab IR, et al. Anterior segment trauma. AAO Basic and Clinical Science Course. Section 8. 1997. 285-6.
- Witherspoon CD, Kunh F, Morris R, et al. Anterior and posterior segment trauma. Master Techniques in Ophthalmic Surgery. 1995. 538-47.
- Tabatabaei A, Kiarudi MY, Ghassemi F, Moghimi S, Mansouri M, Mirshahi A, et al. Evaluation of posterior lens capsule by 20-MHz ultrasound probe in traumatic cataract. Am J Ophthalmol. 2012 Jan. 153(1):51-4. [Medline].
- Kumar A, Kumar V, Dapling RB. Traumatic cataract and intralenticular foreign body. Clin Experiment Ophthalmol. 2005 Dec. 33(6):660-1. [Medline].
- Rofagha S, Day S, Winn BJ, Ou JI, Bhisitkul RB, Chiu CS. Spontaneous resolution of a traumatic cataract caused by an intralenticular foreign body. J Cataract Refract Surg. 2008 Jun. 34(6):1033-5. [Medline].
- Chuang LH, Lai CC. Secondary intraocular lens implantation of traumatic cataract in open-globe injury. Can J Ophthalmol. 2005 Aug. 40(4):454-9. [Medline].
- Phillips PM, Shamie N, Chen ES, Terry MA. Transscleral sulcus fixation of a small-diameter iris-diaphragm intraocular lens in combined penetrating keratoplasty and cataract extraction for correction of traumatic cataract, aniridia, and corneal scarring. J Cataract Refract Surg. 2008 Dec. 34(12):2170-3. [Medline].
- Kumar S, Panda A, Badhu BP, Das H. Safety of primary intraocular lens insertion in unilateral childhood traumatic cataract. JNMA J Nepal Med Assoc. 2008 Oct-Dec. 47(172):179-85. [Medline].
- Shingleton BJ, Hersh PS, Kenyon KR, et al. Lens injuries. Eye Trauma. 1991. 126-34.
Classic rosette-shaped cataract in a 36-year-old man, 4 weeks after blunt ocular injury.
Same cataract as seen in previous image, viewed by retroillumination.
Source...
